“ Transplanted cells produce dopamine in the brain and improve symptoms of Parkinson's disease", says Jun Takahashi, director of the Center for iPS Cell Research and Application (CiRA) at Kyoto University, Japan. In a study led by this stem cell specialist, seven patients with Parkinson's disease were successfully implanted with brand-new dopamine-producing neurons. Published in the same issue of the journal Nature, a second study using another type of stem cells repeats the feat, this time on 12 patients from North America.
Parkinson's disease is caused by the death of dopamine-producing neurons
The seven participants in the Japanese study, aged 50 to 69 and having been ill for more than five years, had not responded to available treatments. In Canada and the United States, the 12 patients were aged 50 to 78 and had been diagnosed for 3 to 20 years. In both studies, the patients were transplanted with dopaminergic neuron progenitors—developing dopaminergic neurons—created by manipulating stem cells. The transplant was performed in the putamen, which is more accessible than the substantia nigra and to which it is connected.
Read alsoResearchers successfully form new neurons in the brains of old mice
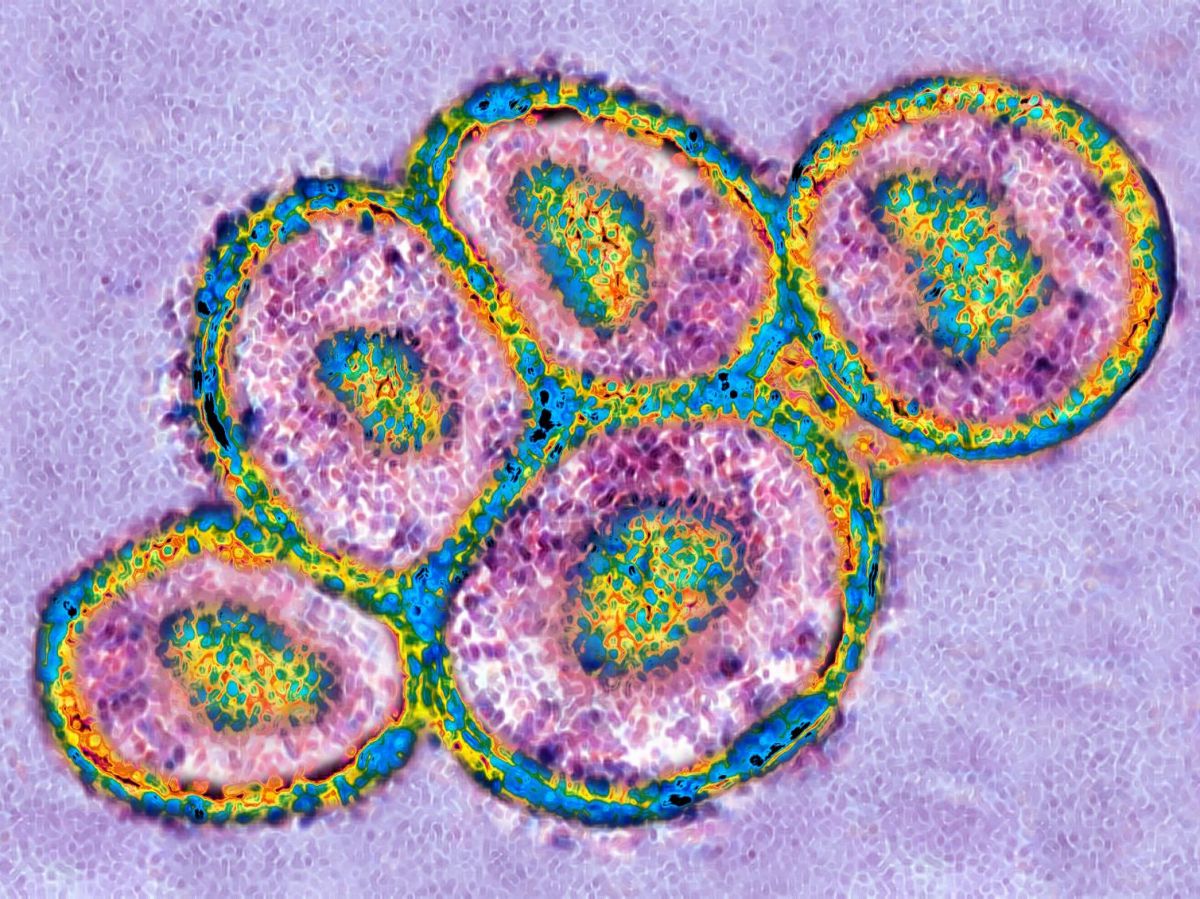
Because in the brain of a Parkinson's patient, it is in this substantia nigra, at the heart of the brain, that certain neurons die prematurely. Without the dopamine that these neurons are responsible for producing, patients gradually experience muscle rigidity, slowed movements, and tremors. Current therapies alleviate the symptoms of Parkinson's disease but do not improve the underlying pathological conditions", points out Jun Takahashi. The main treatment is the drug levodopa, from which the brain produces dopamine. Unfortunately, its effectiveness decreases over time as the population of dopaminergic neurons, capable of converting them into dopamine, decreases. For this reason, researchers have been trying to regenerate dopaminergic neurons themselves since the 1980s.
Using stem cells to create replacement neurons
But several obstacles had to be overcome before arriving at this new work. First, a technique was needed to generate a large quantity of these neural progenitors for transplantation, without having to derive them all from cells found in fetal tissue. In these two new studies, each graft contained one to five million cells depending on the dosage (low or high) chosen. This advancement was made possible through the use of stem cells, cells capable of evolving into any specific cell in the body if given the necessary signals. Here, they were generated using two different methods.
In Japan, these are induced pluripotent stem cells (iPS), genetically reprogrammed in the laboratory from any cell to regress it to the stem cell stage. It was a Japanese researcher named Shinya Yamanaka who earned the 2012 Nobel Prize in Medicine for this discovery. In North America, human embryonic stem cells were used. Initially taken from embryos aged five to seven days but now commercially available, they are capable of multiplying indefinitely.
Read alsoShedding light on Parkinson's disease: a device implanted in the patient's head!
Stem cell therapy that appears safe
The risks were not neutral and included in particular the appearance of dyskinesia (movement disorders) and the development of tumors. For the occurrence of dyskinesias, theOne explanation is the accidental presence of serotonergic neurons in fetal tissue.", explains Jun Takahashi. As for the risk of tumor, it exists in the case of remaining undifferentiated stem cells in the graft.
In the two so-called phase I or II studies, dedicated to evaluating the safety of the product, no significant adverse effects were observed. We knew that iPS cell-derived dopaminergic neurons survived and functioned in the brains of animals (mice, rats, monkeys), but we were uncertain about the human brain.", Jun Takahashi recalls. We have now confirmed the safety of iPS cell-derived dopaminergic neurons in the brains of patients with Parkinson's disease. »
Read alsoResearchers create centenarian cell bank to study secrets of longevity
Although these studies were not designed to evaluate the method's effectiveness, the researchers report initial positive indicators. In the North American study, the graft lasted at least 18 months and reduced 50% symptoms. In the Japanese study, patients also saw almost all their symptoms improve, and in both studies, the researchers confirmed that the graft continued to produce dopamine for up to two years after the operation. The two teams are already planning to move on to the next stage, a phase III clinical study with more patients to evaluate the real-world effectiveness of their products compared to a control group. Today, Parkinson's disease is the second most common degenerative disease in the world (behind Alzheimer's disease), and affects 175,000 people in France.